 |
| Cousins Visiting Gramps in the Hospital |
A good friend of mine who also had struggled with infertility had previously mentioned a fertility clinic to me called the Utah Fertility Center. She knew people who had gone there and had heard positive things about one of the doctors there. So we looked into going to this highly recommended place and made an appointment.
https://www.utahfertility.com/
We started going to the Utah Fertility Center on November 5. We nervously went in for our first appointment, a consultation, with Dr. Gurtcheff. Her warmness and inviting personality helped me feel a little more at ease. She started by getting our background and asking questions to understand why we were there. She asked the typical health questions and recorded our medical history. She noted that I have dysmenorrhea (irregular periods) and a previous diagnosis with PCOS. Side Note: I have since realized that I had never been specifically told my doctors that I have PCOS. I have been told that I have a lot of cysts in my ovaries. So I assumed that meant I had PCOS.
She also asked when my most recent pap smear and physical exam was. She was quite concerned when I told her I hadn't had one for about four years, and she strongly recommended that I have one done as soon as possible. She was also quite concerned when we told her we didn't have insurance, but we told her we were willing to pay out of pocket to get started on the first steps. She warned us that it would be pricey but that she could find ways for us to cut costs.
She went through the different types of tests and treatment options. We opted out of a suggested genetics test but agreed to get a Hysterosalpingogram or HSG for short (a test where they shoot dye through your fallopian tubes to check for blockages) and a test for David. It was also brought up that I had already taken Clomid and that it didn't seem to do anything, so she decided to switch me to another drug called Femara. I was happy with this decision because the same friend who had referred me to the UFC had been successful in getting pregnant when she switched from Clomid to Femara.
We settled on our game plan, had an ultrasound performed, and the doctor sent me to a coordinator to set up my "pre-cycle testing". Most procedures during fertility treatment had to be done at a certain time. Before they could schedule the actual tests and medicine taking dates, we had to wait for my next period to start, and I was instructed to call the center on Cycle Day 1. With a packet full of information and instructions we left the appointment anxiously ready to get things started.
For David, we just had to have an analysis done within 2-4 weeks. We were able to just take in a sample, and the results showed no problems. Wouldn't it be nice if all the tests and procedures had been that easy!
My period started about a week and a half after our consultation in mid-October, and I had an ultrasound a few days later. During the ultrasound appointment I was instructed to start taking my first round of Femara that day and take it for five days. We then scheduled an ultrasound and an HSG for the 26th. As with all medical procedures, I had to fill out a consent form for the HSG. The form indicated the risks and possible complications of the procedure. https://www.asrm.org/FACTSHEET_Hysterosalpingogram/ Talk about freaking a girl out! After reading the form the procedure sounded a bit scary. I was nervous. I spoke to my sister who had also previously had an HSG performed. She helped calm my nerves, and I figured if she had done it and was fine, I would make it through it as well.
The day of the ultrasound and HSG test came. I don't remember if I was more nervous to find out whether or not the medicine worked or for the HSG. First came the ultrasound which showed that my body did not respond to the Femara. I was devastated. I asked the doctor what were we to do now? She said that she would have me do one more round of the medicine at the maximum allowed dosage. If it was unsuccessful then we would have to move up to a more intensive treatment.
Next came the HSG test: the procedure was uncomfortable but not as bad as I had expected. It was a little bit like having a pap smear, there was a little pain and cramping, but it went by quickly. I was able to watch the screen as the process was happening. I remember the Dr. saying that the fluid flowed through both tubes but that one tube flowed a little more slowly. She didn't seem too concerned with this. My medical records even say there was "no intrauterine filling defects noted" and that there was "normal fill and spill of both tubes." At the time I didn't think much of the comment about the fluid moved slower in one tube. I now realize that this may have been more significant than anyone realized, a red flag.
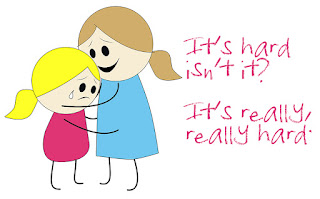
I was so heartbroken when I left the office that day. The thought of having to do IVF scared me. I also knew we couldn't afford to do that yet. If it came down to that then we would have to put the process on hold again. I don't remember if I cried in the office that day after hearing the results but I guarantee I cried in the car on the way home. I remember going over to my sister's house. After telling her the round of medicine was unsuccessful she wrapped me up in a big hug. She said something like, "It's hard isn't it? It's really, really hard."
I don't remember what else she said to me that night but that is all I really needed to hear. Those simple words and warm, comforting embrace told me it was ok to be sad and hurt. It showed me that I wasn't alone and that someone else knew what I was going through. How grateful I was, and still am, to have a sister who knew what to say to comfort me and who understood what I felt because she had walked a similar path. Little did I know that as we stood there in that tender embrace, the storm clouds were slowly gathering and they were dark, full, and threatening.


What a wonderful thing for your sister to say! You're so right! Our greatest need in times like that is just to be understood. I'm so grateful you have her to help you through this!
ReplyDelete